The Complex Dance: Debunking the Simplicity of Posture and Pain
Have you ever caught yourself slouching and immediately thought, "This might hurt later"? We often make an almost instinctual connection between posture and potential pain. But what if the relationship isn't as straightforward as it seems? In this article, we will be delving into the nuanced world of posture and pain, where myths are dismantled and reality, supported by scientific insights, is unveiled.
1. Unraveling the Misconceptions
Every culture, every generation, has its tales, and in the world of physiotherapy, one tale has persisted: “perfect posture equals a pain-free life”. But let's step back and examine this belief under the microscope of scientific research.
1.1 Lack of Evidence
If you've ever thought that the way you're sitting or standing might lead to pain later, you're not alone. It's a common belief shared by a lot. While it's tempting to attribute discomfort and pain solely to one's posture, scientific studies have illuminated a more complex relationship between the two.
For instance, researchers have delved into the connections between posture and pain, and their findings have been illuminating. One compelling study suggests that the direct link between poor posture and pain isn't as straightforward as commonly assumed (1).
This study revealed that pain experiences often depend on various factors, including individual differences in musculoskeletal structures, genetic predispositions, and even psychosocial factors. In some cases, people with seemingly "imperfect" posture may not experience pain at all, while those with "ideal" posture may still grapple with discomfort (1).
1.2 The ‘ideal posture’
The notion of an "ideal posture" is a seductive one. However, real-life studies tell us a different story. When scientists looked at how real people move in their daily lives, they discovered a wide range of what could be considered normal. A study examining lumbar spine alignment in daily situations found that our backs naturally vary in their curve – and this variability doesn't necessarily lead to pain(2). The narrative here is clear: seeking an elusive “perfect” posture may be a wild goose chase.
2. Assessment Challenges
Determining "good" from "bad" posture is like trying to judge a book by its cover. Each person's cover is influenced by countless factors, making judgments tricky and, at times, misleading.
2.1 Challenges of Posture Assessment
Your body is unique, adapting and evolving due to genetics, daily habits, and even emotional states. Trying to fit it into a universally accepted mold of 'good posture' can be challenging. Taking pelvic shape as an example, a study found that individual variations in pelvic morphology are so diverse that pinpointing an "abnormal" posture becomes nearly impossible (3). So, when we talk about assessing posture, it's essential to remember the individuality of each person's body.
2.2 Potential for Bias Assessment
Human judgments come with an array of biases. In the realm of physiotherapy, these biases can have real-world implications. A study on scapular dyskinesis, which is the alteration in the normal position of the shoulder blade, showed that observational assessments can vary based on preconceived notions about what's considered "normal" (4). It's a gentle reminder that every assessment, even scientific ones, can be tinged with personal biases, emphasizing the need for objective evaluation.
3. The Inconclusive Link Between Posture and Pain
The dance between posture and pain is akin to navigating a labyrinth, intricate and multi-layered. We often hear statements like "Sit up straight to avoid back pain," but is it that simple? Delving into scientific research and studies reveals a far more intricate relationship.
3.1 Relationship Complexity
At the crux of our understanding is the realization that posture isn't universally "good" or "bad." A posture that is comfortable and pain-free for one person might cause discomfort to another. This subjective experience becomes evident when examining relationships like lumbar lordosis, pelvic tilt, and abdominal muscle performance. In this study, the variables of lumbar curvature and abdominal strength didn't guarantee a pain-free existence. It highlighted that what might be anatomically normal for one person might not be the same for another, and the way our body structures interact varies tremendously from person to person.
3.2 Avoiding Oversimplification
Simply put, pain is a multifaceted experience. The body is not a mechanical entity where one part malfunctions, leading to a predictable outcome. Instead, it’s an interconnected system where physical, psychological, and environmental factors can all influence our experience of pain. Thus, while posture can play a role, it’s just one of many variables in the equation of pain.
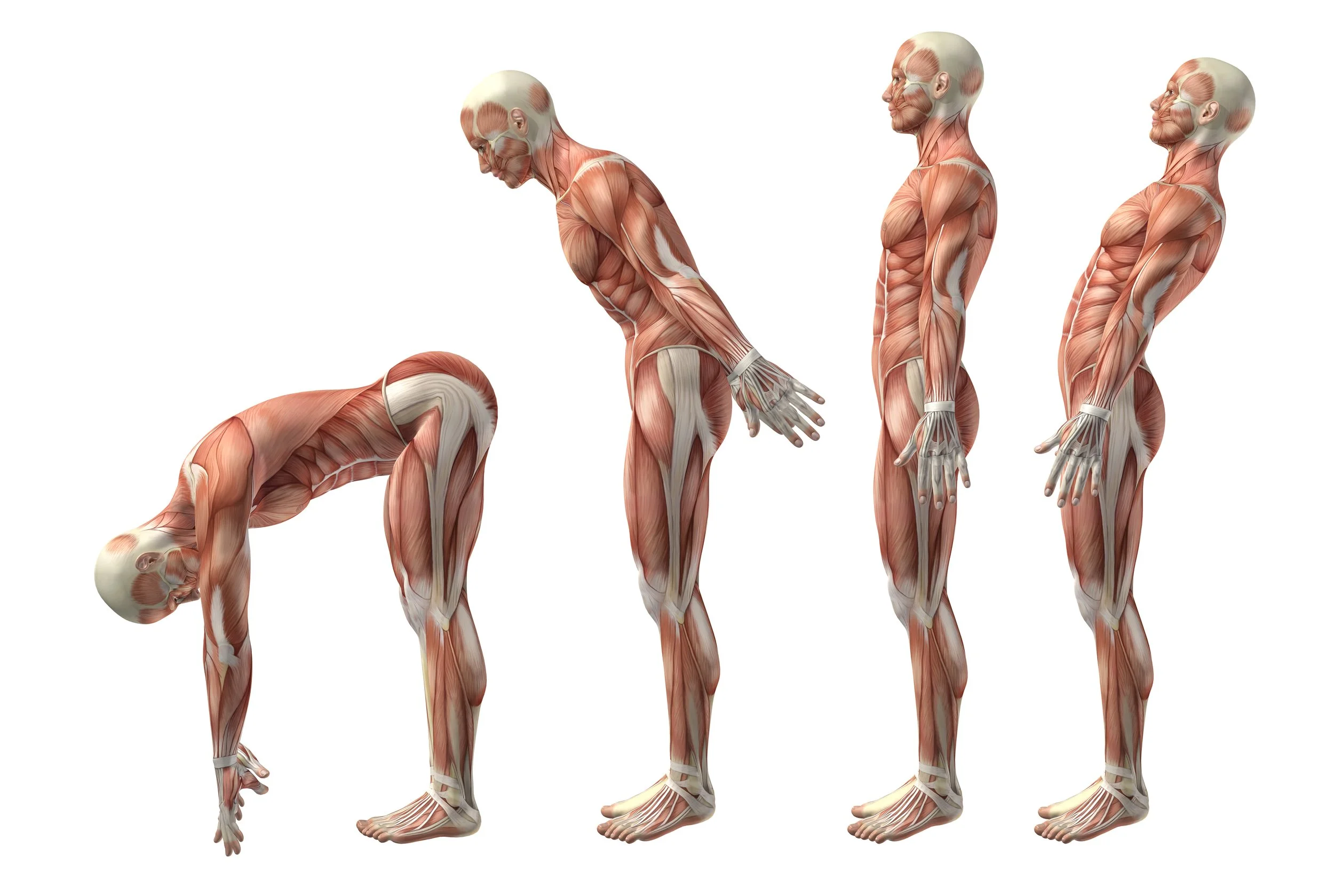
4. The Dynamic Nature of Posture
When discussing posture, we must move away from the notion of a static, unchanging stance. Instead, let's understand posture as a fluid and evolving aspect of our bodily existence, continuously adapting to our environment, tasks, and mood.
4.1 Daily Variations
Have you ever noticed how your posture changes depending on what you're doing? Maybe you slouch a bit while engrossed in a book or stand taller when you're feeling confident. A study comparing postures of asymptomatic subjects and low back pain patients across different phases demonstrates this dynamic change (6). This research found that even in controlled standing positions, there was significant variability between individuals and even within the same individual across different moments. This fluidity underscores the fact that even if there were a “perfect posture,” maintaining it continuously would be an unrealistic expectation.
4.2 Age as a Dynamic Factor
Just as rivers change their course over time, our bodies, too, undergo shifts. One significant factor influencing our posture is age. As we grow older, natural adaptations occur in our muscle mass, bone density, and flexibility. Such changes can and do influence our posture, but it's essential to differentiate between natural age-induced postural adaptations and those that might lead to discomfort or pain. A study on the alignment of the cervical spine in an asymptomatic aging population provides insight into this. The research reveals that while age-related changes in posture are evident, they don't necessarily correlate with pain or discomfort (7). Thus, the idea that “you’re slouching more because you’re getting older” is an oversimplification and doesn't always translate to “you’ll feel more pain as you age.”
5. The Complexity of Pain and Posture Relationship
Our bodies are remarkable systems, interconnected and reliant on various components working in harmony. When pain arises, pinpointing its origin and the contributing factors can be akin to solving a multi-layered puzzle. The relationship between posture and pain encapsulates this complexity.
A common example is the association between hip extension range of motion and postural alignment. On the surface, one might assume a restricted hip extension would directly correlate with specific postural deviations. However, when delved into, the relationship is much more intricate (8).
Imagine someone with restricted hip extension. This could impact their walking pattern, potentially leading to compensatory movements elsewhere in the body. Over time, these compensatory movements might strain other areas, like the lower back or knees. Yet, two individuals with the same hip restriction might develop entirely different compensatory patterns, influenced by their daily activities, muscle strengths, or previous injuries. This underlines the individuality of our bodies and the multifaceted nature of the posture-pain relationship.
Moreover, pain itself is not merely a physical sensation. It's intertwined with our mental state, emotional well-being, and past experiences. An individual's perception of pain can vary widely based on psychological factors, making the relationship between posture and pain even more intricate.
6. Embracing a Holistic Approach
Given the complexities of the posture-pain relationship, a shift towards a more holistic perspective in treatment is paramount. The traditional model that aims to 'correct' posture as a one-size-fits-all solution is being increasingly challenged by emerging research and clinical observations.
Variability in thoracic and lumbar posture behavior in different tasks exemplifies this. For instance, how one sits at their desk while working might differ vastly from their posture when they are relaxed and watching a movie. This change is natural and can even vary significantly among different days or times of the same day (9).
So, what does this mean for treatment? Instead of solely focusing on achieving a 'perfect' posture, practitioners should emphasize functional movement, flexibility, strength, and patient education. Encouraging patients to listen to their bodies, adapt ergonomics to suit their unique needs, and incorporate regular movement breaks can be more beneficial than rigid postural corrections.
Furthermore, the holistic approach goes beyond the physical. Recognizing the influence of psychological and environmental factors on pain can provide a more comprehensive treatment strategy. For instance, addressing work-related stress or ensuring a conducive sleep environment can play a crucial role in pain management.
In essence, this approach acknowledges the individual as a whole, looking beyond mere physical symptoms and posture, to provide a more tailored and effective treatment strategy.
7. Empowering Patients through Education
Understanding our bodies is a fascinating journey. The way we stand, sit, or move can have mysterious interactions with those occasional aches and pains we all feel. However, it’s important to unravel some of the mysteries surrounding posture and pain. Why? Because being well-informed is like having a superpower – it enables us to take charge of our well-being and make choices that enhance our quality of life.
Let’s address a common myth: that there is a ‘perfect’ way to hold ourselves, and if we stray from this magical posture, we’re doomed to a life of discomfort. The truth? Our bodies are marvelous, adaptable machines! There isn’t a one-size-fits-all ‘perfect posture.’ In fact, research and real-life examples show that what works wonders for one person might not work the same way for another.
Moreover, it’s essential to acknowledge that pain is like a puzzle, with many pieces coming together. It’s not just about how we sit or stand but also about our environment, our mental state, our lifestyle, and so much more. Realizing this helps us see the bigger picture and enables us to approach our well-being more holistically.
So, what does this mean for you? It’s about embracing the uniqueness of your body, being mindful of its signals, and recognizing that there are various factors at play when it comes to pain. Armed with this knowledge, you become an active participant in your journey towards feeling your best. And remember, your healthcare provider is your ally, ready to guide you and address your questions, making the journey less daunting and more enlightening.
BUT DO WE CLINICIANS STILL ADVISE ON POSTURE?!
Actually, YES, we do! Postural, ergonomic and even movement alterations can still be used to specifically offload injured or irritated structures and are in fact very powerful. We use this often in the neck, low back and hip. This does not mean however that every patient needs to sit or stand the same way. This individual advice follows an understanding of the exact structural irritation that may be occurring and the mechanics of offloading it and for how long that may need to be for!
The human body is a marvel, and our posture is just one aspect of this incredible machine. While it's tempting to believe there's a one-size-fits-all solution to pain related to posture, the truth is much more nuanced. Studies, experts, and real-life experiences all point to one conclusion: the relationship between posture and pain is complex and deeply individual.
So, the next time you hear someone mention the importance of "sitting straight to avoid pain," remember that the story isn't that straightforward. Instead, focus on understanding your body, being mindful of how you feel, and seeking expert advice when in doubt. Your body is unique, and understanding its signals is the first step towards a comfortable, pain-free life.
References
Wernli, Kevin & O'Sullivan, Peter & Smith, Anne & Campbell, Amity & Kent, Peter. (2020). Movement, posture and low back pain. How do they relate? A replicated single‐case design in 12 people with persistent, disabling low back pain. European Journal of Pain. 24. 10.1002/ejp.1631.
Differences between clinical “snap-shot” and “real-life” assessments of lumbar spine alignment and motion – What is the “real” lumbar lordosis of a human being? https://www.sciencedirect.com/science/article/abs/pii/S0021929016300586
Variation in pelvic morphology may prevent the identification of anterior pelvic tilt https://pubmed.ncbi.nlm.nih.gov/19119397/
Observational Scapular Dyskinesis: Known-Groups Validity in Patients With and Without Shoulder Pain https://www.jospt.org/doi/full/10.2519/jospt.2017.7268?code=jospt-site
Relationships between lumbar lordosis, pelvic tilt, and abdominal muscle performance https://pubmed.ncbi.nlm.nih.gov/2951745/
How do we stand? Variations during repeated standing phases of asymptomatic subjects and low back pain patients https://www.sciencedirect.com/science/article/abs/pii/S0021929017303135
The change of cervical spine alignment along with aging in asymptomatic population: a preliminary analysis https://link.springer.com/article/10.1007/s00586-017-5209-1
Relationship between Hip Extension Range of Motion and Postural Alignment https://www.jospt.org/doi/pdf/10.2519/jospt.1990.12.6.243
Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements https://www.sciencedirect.com/science/article/abs/pii/S0003687015300788