Discs Can Suffer Injuries, But Their Capacity To Heal Is Undeniable
In the digital age, where quick fixes and instant solutions are often sought after, the resilience and regenerative capacity of the human body still amaze us, particularly when it comes to our spinal discs. The notion that "discs can suffer injuries, but their capacity to heal is undeniable" offers a refreshing perspective on spinal health, moving away from fear-inducing beliefs towards a more hopeful and science-backed understanding. This article aims to demystify common misconceptions about disc injuries, enlighten readers with the latest scientific findings, and inspire those suffering from disc-related issues with a message of hope.
Understanding Disc Injuries
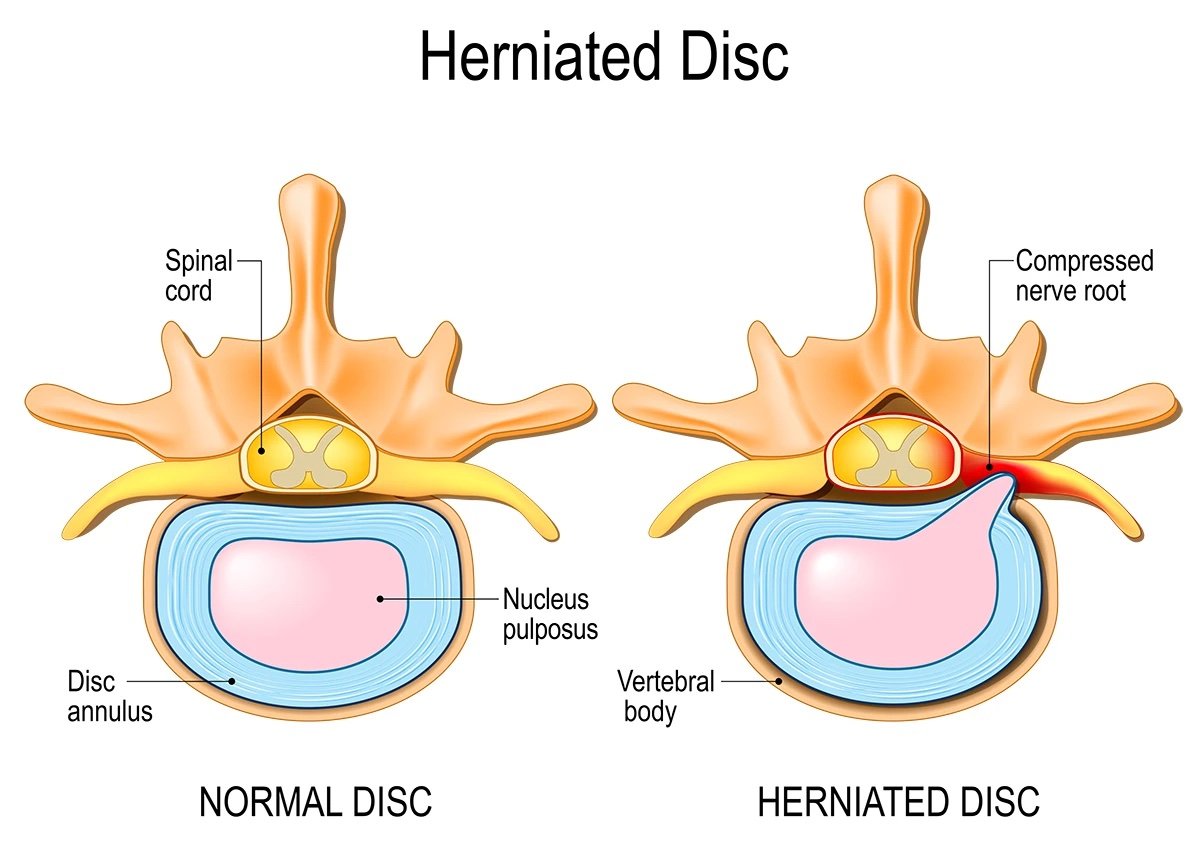
Disc injuries are typically the result of degenerative changes over time or acute injury, arguably from improper lifting, sudden movements, or trauma. These injuries can lead to conditions such as herniated discs, where the inner gel-like core (nucleus pulposus) protrudes through a tear in the outer ring (annulus fibrosus), potentially irritating nearby nerves. Symptoms can include pain, numbness, and weakness along the nerve's path, such as in the case of sciatica, which affects the sciatic nerve running from the lower back down the legs .
The Myth of the Slipping Disc
One of the most pervasive myths in spinal health is the concept of the "slipping disc." This term misleadingly suggests that discs, which sit between the vertebrae, can slide out of place, causing pain and discomfort. However, this is a misconception. Spinal discs are securely anchored. They essentially act like ligaments connecting bone to bone and cannot simply "slip" out of position. They can, however, suffer from tears, bulges, and degeneration, which are the actual sources of pain, not the displacement of the disc itself .
Debunking the Sciatica Myths
Sciatica, often associated with disc herniations, is characterized by pain that radiates along the path of the sciatic nerve. The link between sciatica and disc injuries has been clouded by myths, including the inevitability of surgery and the ineffectiveness of conservative treatments. However, studies have demonstrated that physical therapy, exercise, and patience can be as effective as surgery in managing sciatica, with the added benefits of lower risks and fostering the body's natural healing processes . Of course, if neurological symptoms such as numbness or weakness are progressing or not improving or there are other red flags then surgery is an option but a good physiotherapist will monitor this and refer appropriately.
The Science of Healing
Discs, despite being subjected to daily stress and strain, have a remarkable ability to heal and regenerate. Contrary to the belief that they are avascular structures doomed to degenerate over time without any hope of recovery, recent research has shed light on their intrinsic healing capabilities. The process of disc healing is complex and involves the migration of cells to the site of injury, proliferation, and synthesis of extracellular matrix, allowing the disc to repair itself over time . In fact there is some evidence that the bigger the disc injury the greater the healing that takes place as viewed on MRI scans one year post.
Physical Therapy and Exercise
Physical therapy and exercise are often the first line of defense against disc injuries. These non-invasive treatments focus on pain management techniques, strengthening the muscles that support the spine, improving flexibility, and reducing the strain on the discs. For conditions like sciatica, where nerve pain can be debilitating, physical therapy aims to alleviate pressure on the nerve through targeted exercises. Techniques such as manipulation, dry needling and electrotherapeutic modalities can then be used as adjuncts to support pain relief and potentially allow for the movement that will support healing.
The Role of Patient Education and Mindset
Patient education and mindset play a significant role in the recovery process. The language healthcare professionals use when discussing spinal health can have a profound impact on patient outcomes. Studies have found that patients who understand their condition and the natural history of disc healing are more likely to engage in positive health behaviors and experience better outcomes .
Surgery vs. Conservative Management
While surgery is an option for severe disc injuries that do not respond to conservative treatment, it is generally considered a last resort. A systematic review found that for many cases of sciatica, conservative management, including physical therapy and exercise, can be as effective as surgery in the long term . This fact alone demonstrates the body's capacity to heal itself with the proper support and interventions. Of course as discussed there may be times when surgery does become the pereferred option but your physiotherapist should be able to counsel you appropriately if that time comes.
In Summary….
The narrative surrounding spinal discs and their ability to "slip" has long been debunked, yet it persists in the collective consciousness. Discs can indeed suffer injuries, but they are firmly held in place, and their capacity to heal is undeniable. Through a combination of physical therapy, exercise, patient education, and, when necessary, advanced treatments, most individuals can recover from disc injuries and lead healthy, active lives.
Our understanding of the spine is continually evolving, and with it, our approach to managing spinal health. By focusing on the body's inherent healing abilities and supporting this process through evidence-based treatments, we can change the discourse on spinal care from one of fear and misunderstanding to one of hope and resilience.
References
Schmid, A., Fundaun, J. and Tampin, B., 2020. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management.
Goldsmith, R., Williams, N.H., Wood, F., 2019. Understanding sciatica: illness and treatment beliefs in a lumbar radicular pain population. A qualitative interview study.
Fernandez, M., Ferreira, M.L., Refshauge, K.M., Hartvigsen, J., Silva, I.R.C., Maher, C.G., Koes, B.W., Ferreira, P.H., 2016. Surgery or physical activity in the management of sciatica: a systematic review and meta-analysis. European Spine Journal 25, 3495–3512
Di Mattia, F., Tejani, S. and Hall, T., 2018. Bed Rest for Sciatica: A Closer Look at the Evidence. Journal of Orthopaedic & Sports Physical Therapy, 48(6), pp.436-438.
Dedering, Å., Peolsson, A., Cleland, J.A., Halvorsen, M., Svensson, M.A., Kierkegaard, M., 2018. The Effects of Neck-Specific Training Versus Prescribed Physical Activity on Pain and Disability in Patients With Cervical Radiculopathy: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation 99, 2447–2456.
Park, J., Lee, Y., Lee, Y., Shin, S., Kang, Y. and Koo, K., 2020. Deep gluteal syndrome as a cause of posterior hip pain and sciatica-like pain. The Bone & Joint Journal, 102-B(5), pp.556-567
Jesson, T., 2020. Sciatica. The Clinicians Guide. Book 1, What is it?
Biomechanical properties of human thoracic spine disc segments https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2944859/#CIT16
The enduring impact of what clinicians say to people with low back pain https://pubmed.ncbi.nlm.nih.gov/24218376/